Symptoms don’t always show up the same way every time
A bite feels harmless. A few minutes pass. Then itching. Swelling. Maybe a rash. Maybe hives. But sometimes, nothing happens until hours later. The stomach tightens. Cramping begins. Breathing feels shallow. Food allergies don’t follow a script. They shift. They surprise. They catch you when you least expect it.
Some people feel it in their throat. Others in their skin. Some feel it everywhere. One food can trigger mild symptoms in one moment, then cause anaphylaxis the next. That’s what makes it hard. It’s not just what you eat. It’s when. How much. And how your body decides to react.
No two reactions are identical—even to the same food.
Common triggers aren’t always obvious in the ingredient list
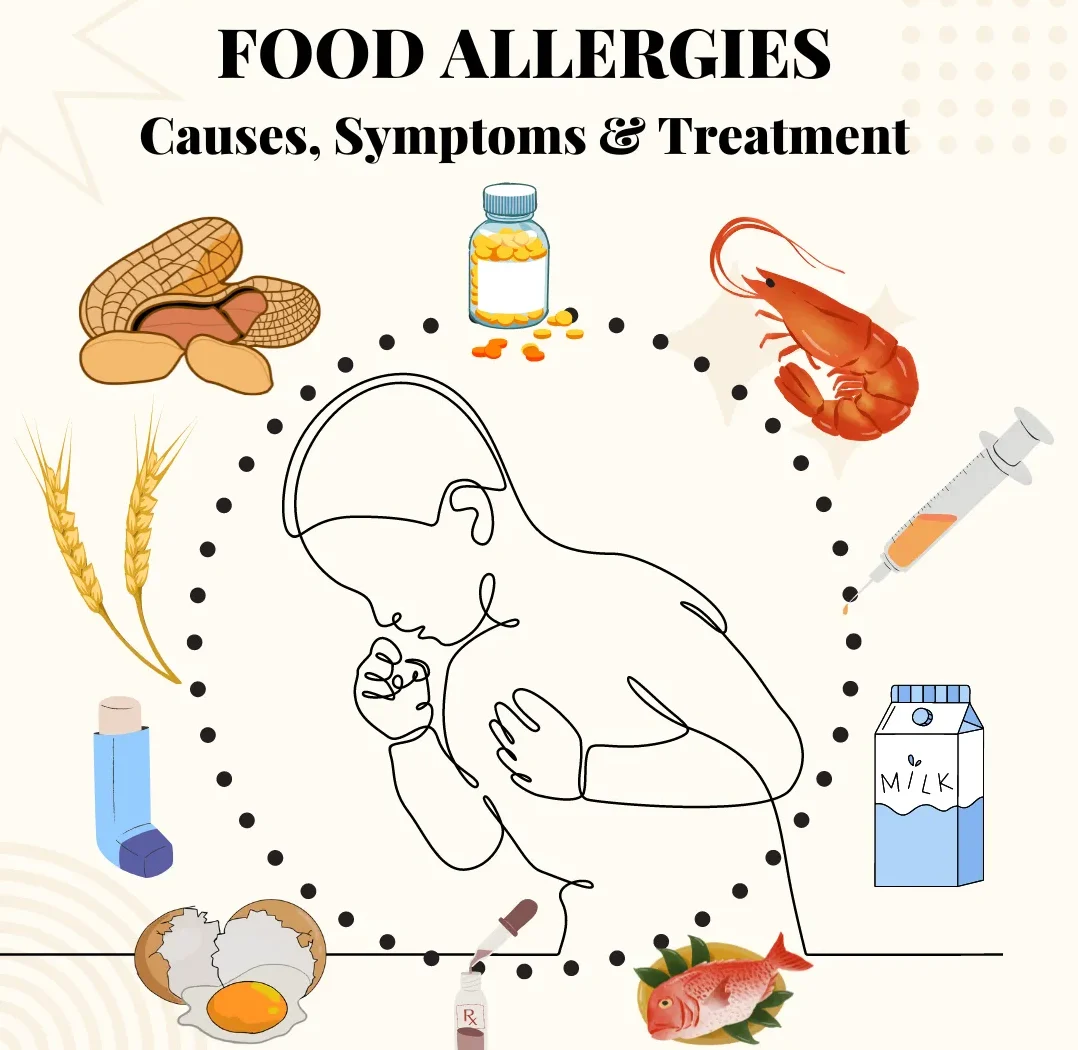
Peanuts. Tree nuts. Milk. Eggs. Shellfish. Fish. Soy. Wheat. These are the major allergens. But they show up in unexpected places. In sauces. In dressings. In baked goods. Under different names. Cross-contaminated on shared surfaces. Hidden in flavorings.
Sesame has become a rising concern. So has lupin. And for some, fruits and vegetables trigger reactions—especially when raw. That’s called oral allergy syndrome. It feels like tingling. Like itching. Like a mild irritation that shows up after fresh produce.
The trigger isn’t always the food itself. It’s how it was processed. How it was handled. What it touched before it reached your plate.
Reactions can be fast—or dangerously delayed
Some symptoms happen within minutes. Sneezing. Swelling. Vomiting. But some take hours. That’s especially true for conditions like Food Protein-Induced Enterocolitis Syndrome (FPIES), mostly in children. It causes delayed vomiting. Diarrhea. Lethargy.
Anaphylaxis is the most serious form. It affects breathing. Blood pressure. Consciousness. It can start with just a mild itch—or jump directly to airway swelling. That’s why people carry epinephrine. Because the early signs aren’t always loud. But the outcome can be.
Never assume a reaction will be like the last one. That’s how allergies become emergencies.
Testing helps—but doesn’t always give clear answers
Skin prick tests. Blood tests. Elimination diets. Food challenges. Each method offers clues. None are perfect. A positive result doesn’t always mean danger. A negative test doesn’t always mean safety.
Some people test positive for dozens of allergens—and react to none. Others test negative, then still get symptoms. That’s because allergies involve the immune system. And immune systems are messy. They respond to more than just exposure. They respond to context.
A trained allergist makes sense of the numbers. Patterns matter more than single results.
Children sometimes grow out of allergies—but not always
Milk. Egg. Soy. Wheat. These are common in early childhood. Many outgrow them by age five. But not all. Peanut and tree nut allergies are more persistent. Shellfish and fish often stay for life. There’s no simple test to tell who will outgrow and who won’t.
Introducing allergens early, under guidance, can sometimes help. Delaying isn’t always better. But the decision should come from a specialist. Not a guess. Not a blog.
Allergies change—but they rarely vanish overnight.
Management is about awareness, not fear
Living with a food allergy doesn’t mean avoiding life. It means learning. Reading labels. Asking questions at restaurants. Telling others. Carrying medication. Having a plan. It’s not always easy—but it becomes habit.
Some learn to bake at home. Others bring snacks to events. Children learn to speak up. Adults learn to ask twice. It’s not about living in fear. It’s about understanding your body—and protecting it quietly, daily.
The hardest part is trusting that the world will take you seriously. That’s why clear labeling matters. Why education helps. Why support is more than just recipes.
Cross-contact makes safe foods unsafe
It’s not just what’s in the dish. It’s what touched the dish. Shared fryers. Reused knives. Unwashed hands. That’s cross-contact. And it’s how even allergy-friendly foods become dangerous.
In bakeries. In restaurants. In schools. Even at home. One speck of peanut butter in a jelly jar. One splash of milk on a cutting board. It doesn’t take much. That’s why allergy protocols matter. That’s why clear kitchens save lives.
Avoidance isn’t paranoia. It’s precaution.
Allergy vs. intolerance—they’re not the same
Lactose intolerance causes bloating. Discomfort. Gas. But it doesn’t involve the immune system. It’s not an allergy. The same goes for gluten sensitivity in people without celiac disease. It’s real—but it’s not life-threatening.
Food allergies involve IgE antibodies. The immune system treats the food like danger. That’s why the reactions can be immediate. Severe. Unpredictable.
Confusing the two leads to misunderstanding—and missed safety.
Epinephrine is the first line—not the last resort
If you’re prescribed an epinephrine auto-injector, use it. At the first sign of a serious reaction. Not when it’s “really bad.” Not after the second symptom. Delaying makes it worse. Faster is safer.
Antihistamines don’t replace epinephrine. They treat hives, itching. They don’t stop airway swelling. They don’t prevent shock. They’re supportive—not protective.
If in doubt, inject. You won’t regret acting early—but you might regret waiting.
Food allergies reshape routines—but not identity
You’re not fragile. You’re not difficult. You’re informed. Prepared. Capable. Food allergies may shift what you eat. But not who you are. You can dine out. Travel. Celebrate. Thrive. It just takes planning.
Support makes that easier. At school. At work. In relationships. Understanding replaces judgment. That’s where safety grows—from shared awareness, not silent worry.
You learn. Others learn. And together, life continues—one safe bite at a time.
